Coronavirus (COVID-19): Guidance for Patients – March 2019
Safety of patients and staff is paramount at this time with the evolving situation around the Coronavirus (COVID-19). I want to reassure my current and potential patients that the hospitals I work at are taking the developing situation very seriously. We are following the guidance from the Department of Health and the Royal College of Ophthalmologists.
Measures to help protect our patients, clinicians and staff include:
- Calling people ahead of their medical appointments at all hospitals and medical centres to check if they have any symptoms. If they have any symptoms they will be advised to self-isolate, following government advice.
- All staff, patients, visitors, contractors and Consultants will be asked to consent to having their temperature taken at reception area before being granted access to the hospital. Anyone that does not consent or has a temperature of over 37.8 degrees will not be granted access and asked to return home and self-isolate
- Advising patients to come on their own unless they need assistance from family or friends
- Encouraging visitors to stay in the car or away from the clinic while waiting
- Maintaining a safe distance between patients in waiting and sub-waiting areas
- Advising all visitors to use hand gel and/or wash their hands upon arrival
- All staff wash their hands on arrival for 20 seconds and use hand gel and/or handwashing after every patient contact
- Cleaning of all points of contact by patients following examination
- Installation of a cough guard at the Slit lamp microscope to protect patients and staff during examination at close proximity
Some consultations may be possible over the phone / FaceTime – please contact my P.A. to arrange this.
The NHS is the best place to seek the latest medical advice.
Presentation at the Brighton Meeting “High risk ptosis surgery” – October 2018
Thank you to Saul and Mayank for organising this wonderful day. My talk included tips for those patients who could miss out on beneficial surgery otherwise!


New publication in Eye – September 2018
Long-term outcome of flexible onabotulinum toxin A treatment in facial dystonia
New publication from the team in Eye reporting our long-term outcomes of onabotulinum used to treat facial dystonia and compare a flexible and fixed treatment regimen.
Clinical Excellence Award – April 2017
The Clinical Excellence Awards (CEA) scheme is intended to recognise and reward those consultants who contribute most towards the delivery of safe and high quality care to patients and to the continuous improvement of NHS services including those who do so through their contribution to academic medicine.
I am delighted to say I have received a 2017 award!

Thank you to the team and all those who continue to strive for their patients at QVH!
Andre.
These awards are made to consultants who:
- demonstrate sustained commitment to patient care and wellbeing or improving public health
- sustain high standards of both technical and clinical aspects of service while providing patient-focused care
- in their day-to-day practice demonstrate a sustained commitment to the values and goals of the NHS by participating actively in annual job planning, observing the private practice code of conduct and showing a commitment to achieving agreed service objectives
- through active participation in clinical governance contribute to continuous improvement in service organisation and delivery
- embrace the principles of evidence-based practice
- contribute to knowledge base through research and participate actively in research governance
- are recognised as excellent teachers and or trainers and or managers
- contribute to policy-making and planning in health and healthcare
- make an outstanding contribution to professional leadership.
Publication in Ophthalmic Plastic and Reconstructive Surgery – March 2017
Can we improve the tolerance of a false eye by enhancing its surface finish?
 Our new publication in Ophthalmic Plastic and Reconstructive Surgery, has advance proofs available online now.
Our new publication in Ophthalmic Plastic and Reconstructive Surgery, has advance proofs available online now.
People who wear an ocular prosthesis frequently suffer with dry eye symptoms and socket discharge, often on a daily basis. In this randomized controlled trial, we used an enhanced polish of the false eye (using aluminum oxide) to achieve a smoother surface. This resulted in reduced deposit build up and less discomfort at 12 months.
Access to the full article is available through the link above.
Publication in Ophthalmic Plastic and Reconstructive Surgery – July 2016
The Effect of Manuka Honey on Eyelid Healing
New publication from the team in Ophthalmic Plastic & Reconstructive Surgery reporting our prospective randomized controlled trial on the effects of Manuka honey on eyelid surgical wound healing.
Fifty-five patients undergoing bilateral upper blepharoplasty were randomized so that one eyelid received Manuka honey twice daily. The eyelids were then graded by two observers at 1 week, 1 month, and 4 months using Manchester scar scale and a modified eyelid scar grading scale.
We found a trend toward less distortion of the surrounding skin and the scar being less palpable on the Manuka-treated side. Patients reported the scar on the Manuka side to have less stiffness (p = 0.058). At 4 months, scar grading scales showed no differences; however, patients reported scar pain to be significantly less on the Manuka-treated side than control (p = 0.005). Thirty-one of the 46 patients believed the scars were similar on both sides, 11 preferred the honey-treated side, and 4 preferred the control.
In conclusion we feel that Manuka honey may provide subjective benefits in the early postoperative period.
Royal College of Ophthalmologists National Congress – 24 May 2016
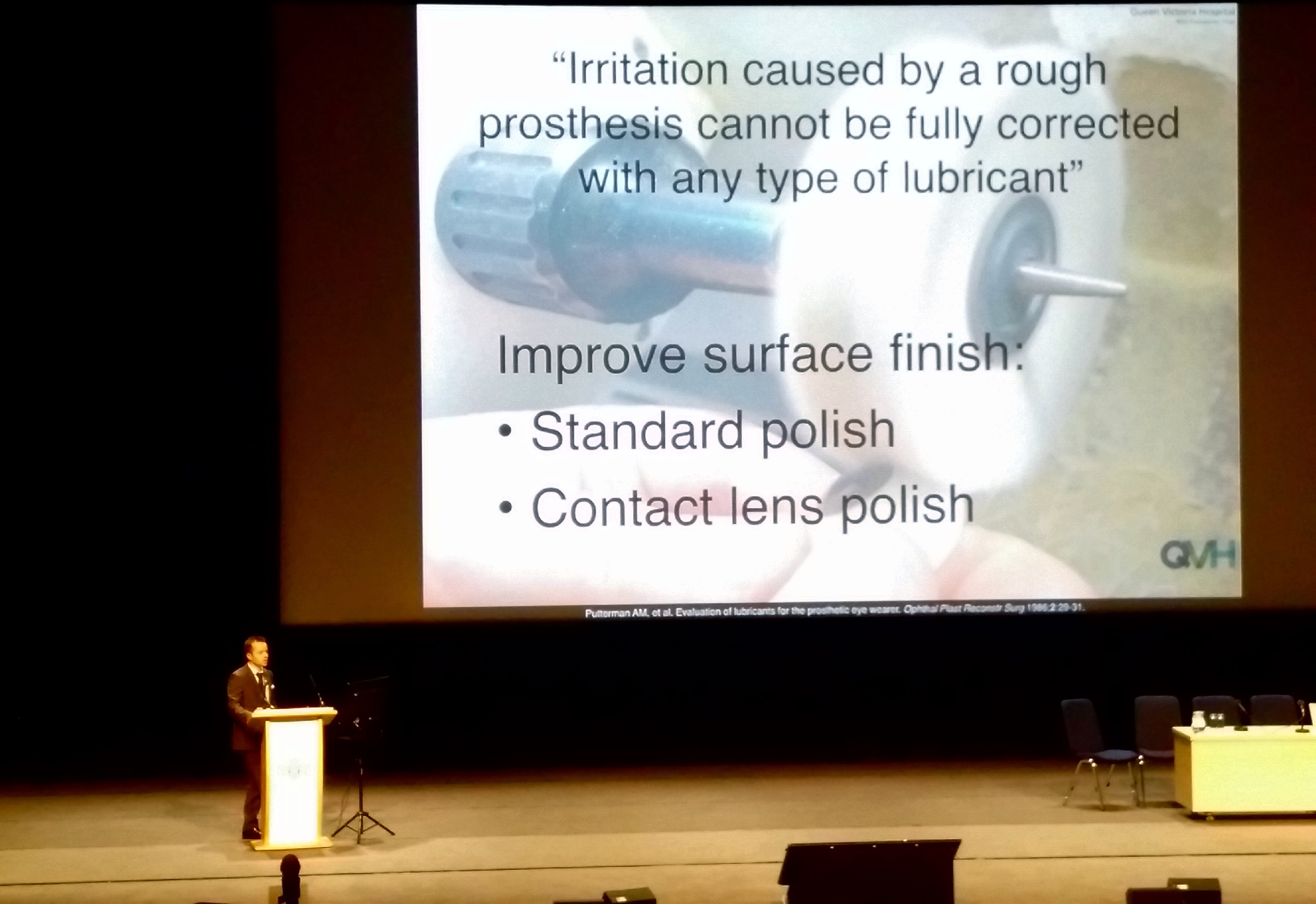
I presented our recent work on smoother artificial eyes (ocular prosthetics) at the National Congress of The Royal College of Ophthalmologists in Birmingham.
In this prospective single-blind randomised controlled trial, we found the enhanced polishing of ocular prostheses using aluminium oxide achieved a smoother surface, resulting in reduced deposit build up and less patient-reported discomfort.
It has now been submitted for peer-reviewed publication also!
Details below…
Participants were randomised to either a standard, or a higher ‘optical quality’ polish of their prosthesis. At entry to the trial and at 1 month and 12 months they completed a questionnaire covering cleaning, lubricant use, inflammation, discomfort and discharge. Lower scores indicated better tolerance of the prosthesis. At each visit, the prosthesis was stained and photographed against a standard background to assess deposit build up.
41 patients participated in the study. The median age of their prosthesis was 36 months (range 9 months to 40 years). There was no statistically significant difference in questionnaire scores or deposit build up between the two groups at baseline. By 12-months, the higher optical quality polish showed a statistically significant reduction in symptoms and frequency of discharge (2.19 v 3.85; p = 0.05 – lower scores better). Scoring of the prosthesis’ deposit build-up showed a significant difference at 1 month, but this was not sustained at 12 months.
Creating an optical quality finish to an ocular prosthesis reduces deposit build up on artificial eyes and improves patient tolerance.
Publication in Ophthalmic Plastic and Reconstructive Surgery – March 2016
Facial fat grafting for people with facial palsy
Recently accepted for publication in Ophthalmic Plastic and Reconstructive Surgery. We have shown that autologous fat grafting is an effective procedure for restoring symmetry and improving eye closure in individuals with facial nerve palsy. Overall, patient-satisfaction was shown to be high and patients would recommend this treatment to others. Future studies with longer follow-up will be required to assess the longevity of the grafted fat and its effectiveness on clinical outcomes.

Publication in the British Journal of Ophthalmology – September 2015
CADS grading scale: towards better grading of ophthalmic involvement in facial nerve paralysis
Our group has published validation of a facial nerve grading scale specifically designed for ophthalmic assessment of facial nerve paralysis. This has been developed and used, to standardise the doctor’s assessment of involvement and to grade surgical outcomes in the rehabilitation of this cohort of patients.
Link to the full-text at http://bjo.bmj.com/content/early/2015/10/15/bjophthalmol-2015-307167.abstract
New publication in the British Journal of Ophthalmology – May 2015
Platinum segments for upper eyelid loading
Congratulations to our group on the publication of our experience using platinum segments for upper eyelid loading in 18 patients. Platinum segment provide the benefits of platinum chains with additional advantages of postoperative adjustability. They can be used as an addition to pre-existing in situ weights or chains.
Link to the full-text at http://bjo.bmj.com/content/early/2015/05/17/bjophthalmol-2015-306869.abstract?sid=20e17256-b9a8-4b91-bb51-e7fe94f866ca
Two chapters in Yanoff’s Expert Techniques in Ophthalmic Surgery – February 2015
I am delighted to announce I will have two Chapters published in Yanoff’s Expert Techniques in Ophthalmic Surgery when it is released next month. This is a comprehensive ophthalmic textbook with almost 1000 illustrations and images. It is available to pre-order from all good bookshops, please see the Amazon here.
Both chapters appear in Section 6 – Oculoplastic, Orbital and Lacrimal Surgery:
Periocular Fillers – Chapter 59
The last 10 years have witnessed a revolution in the field of cosmetic surgery. The current top nonsurgical cosmetic procedures are botulinum toxin injections and hyaluronic acid fillers. This is a dramatic change from 15 years ago when the majority of aesthetic procedures were surgical.
Volume loss has increasingly been recognised as an important aspect of facial aging and this is especially true of the periocular region. Soft tissue augmentation has therefore become a vital component of facial rejuvenation.
Ptosis Repair (Internal Approach Levator Surgery) – Chapter 64
The newer techniques of posterior approach levator advancement are now an option in the majority of patients with ptosis and moderate to good levator function, even in phenylephrine negative cases.
A non-excisional, conjunctival approach allows for a rapid healing process whilst avoiding the need for a skin incision.
Please contact me if you would like any further details, I am looking forward to seeing the rest of the book!
Brighton – The Argus January 15 2015
First publicity of the year on the use of Coleman fat transfer in rejuvenating the eyelids and mid-face. Based on my forthcoming chapters in Yanoff’s Expert Techniques in Ophthalmic Surgery (Jaypee Brothers Medical Publishers 2015).
As we age, everyone’s face loses some of its youthful plumpness. This is especially true around the eyes. Simply replacing this lost fat can take years off a person’s perceived age.
To read the article in full please click here.
First peer-reviewed publication of the year in the British Journal of Ophthalmology – January 2015
Blepharoptosis surgery in patients with myasthenia gravis
Myasthenia gravis is typically an acquired muscle weakness (derived from the Greek word ‘myasthenia’and the Latin word ‘gravis’ meaning ‘serious’). Droopy eyelids (blepharoptosis) and double vision (diplopia) are common manifestations, with approximately half of all patients first presenting to an Ophthalmologist. This paper reviews 30 patients with eyelid concerns despite appropriate medical treatment, who required eyelid surgery.
Link to the full-text at http://bjo.bmj.com/cgi/content/full/bjophthalmol-2014-306335
The Great Debate: External Versus Endonasal Dacryocystorhinostomy
Exciting news! I just found another of my books is now in print! I wrote the above chapter with my QVH colleague Raman Malhotra, for Javed Ali’s book: Principles and Practice of Lacrimal Surgery. Please see the publisher’s website for further details:
Link to the full-text at http://www.springer.com/medicine/ophthalmology/book/978-81-322-2019-0
Lacrimal disorders are very commonly encountered not only by the Oculoplastic surgeons but also by the general Ophthalmologists and Optometrists in their daily practice.
In Chapter 38 we review how far surgery for blocked tear ducts has come since twelfth-century Andalusian Oculists used small spear-shaped instruments to perforate the lacrimal bone into the nose. The probe was then wrapped in cotton and soaked in ox fat. It was exchanged every day in order to maintain the patency of the created fistula – a similar underlying principle remains today.
It has recently been accepted that skin incision (external) or endonasal (endoscopic surgery within the nose) approaches to blocked tear ducts are equally successful. The chapter reviews both methods of dacryocystorhinostomy (or DCR for short) and finds that many surgeons still prefer and perform greater numbers of external procedures. Is the tide turning however? Approaches to DCR surgery may no longer represent such a great debate, but a division of experience and training between generations of surgeons, with a younger generation increasingly performing endoscopic (no skin incision) surgery.